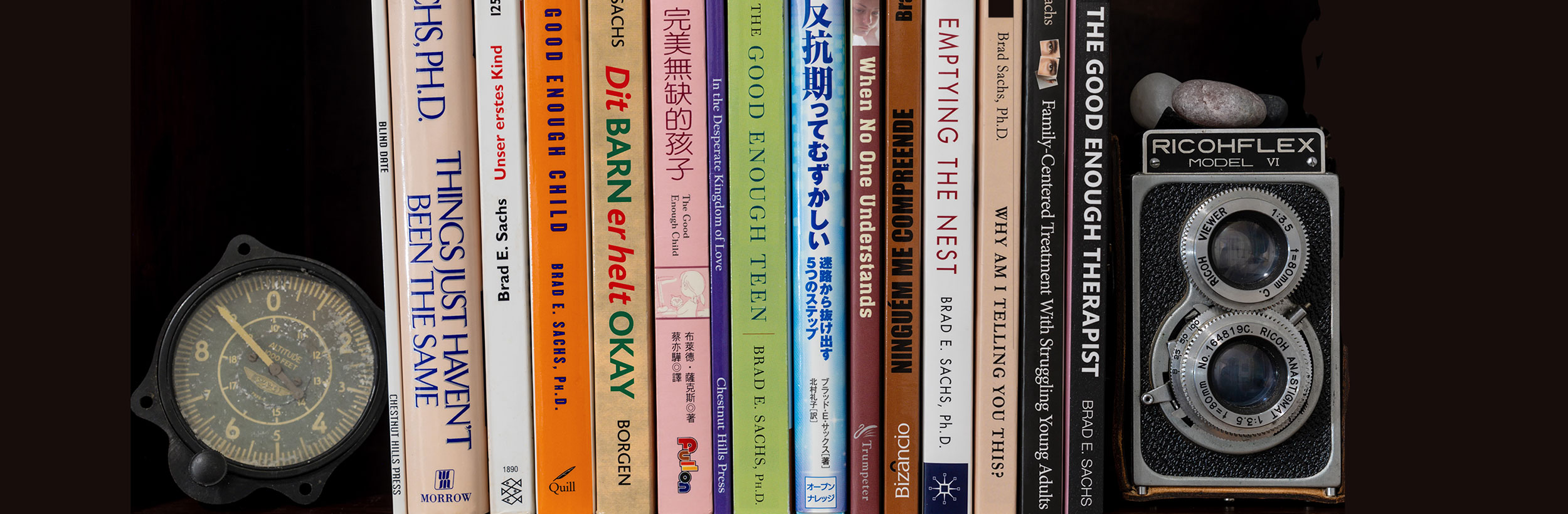
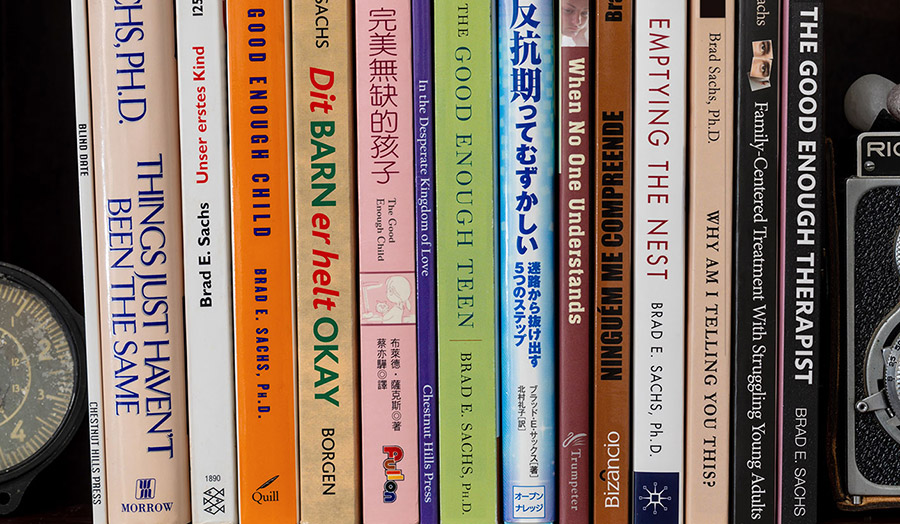
I am a best-selling, award-winning author who has published 10 books, some for general readership and others for professional readership. Many have been translated into multiple languages.
I write because it helps me to understand what I have learned from my patients, and because I want to share those lessons with a wider audience.
The Good Enough Teen
Raising Adolescents with Love and Acceptance (Despite How Impossible They Can Be)
(HarperCollins)
When No One Understands
Letters to a Teenager on Life, Loss, and the Hard Road to Adulthood
(Shambhala)
Things Just Haven't Been the Same
Making the Transition from Marriage to Parenthood
(William Morrow)
Family-Centered Treatment With Struggling Young Adults
A Clinician's Guide to the Transition From Adolescence to Autonomy
(Chestnut Hills Press)